There are 3 main ways that breathing support can be given in ICU.
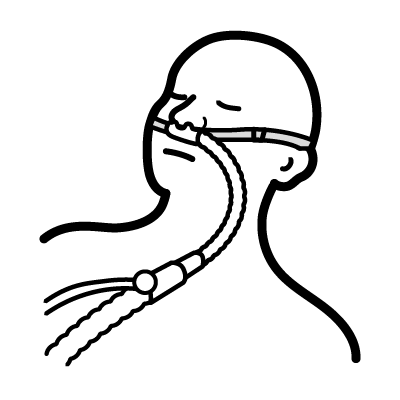
This is for patients who are breathing on their own. A device in their nose is attached to oxygen mixed with warm and humidified air. The oxygen is delivered in high-flow and can be given at high levels.
Some patients receive breathing support through a mask. These patients are breathing for themselves. The support helps to lesson the effort of breathing. This type of breathing support is called “non-invasive ventilation”.
The mask is strapped on tight over the nose and mouth. This is to create a seal so that air and oxygen can be given with pressure to the lungs. It is hard for patients to talk (and be heard) with the mask on. It can also dry out the mouth. Nurses will take the mask off for short breaks when it is safe to do so.
Some people use machines at home called CPAP machines to help them breathe at night. The machine used in ICU is similar but can deliver stronger pressure and oxygen.
The machine can be set to give continuous pressure to the airway (CPAP). It can also be set to give higher pressure on the “in-breath” and a lower pressure on the “out-breath” (BiPAP).
Breathing support given through a breathing tube is called “invasive ventilation”. Patients needing a breathing tube require a ventilator (breathing machine) to breathe for them. Two types of breathing tubes are the endotracheal tube (ETT) and a tracheostomy tube.